Share
Fighting Hospital Acquired Infections
Author
Ashish Taneja, Lab Leader-Home and Industrial & Institutional CleaningPublished On
November 18, 2019Author
Ashish Taneja, Lab Leader-Home and Industrial & Institutional CleaningPublished On
November 18, 2019Share
Markets
- Institutional Cleaning & Sanitation
Related Products
Fighting Hospital Acquired Infections – How cleaning products can be designed to help hospitals fight healthcare-associated infections.
Hospitals and other health care institutions are constantly working to prevent health care associated infections (HAIs). According to a study by the Centers for Disease Control and Prevention (CDC), at any given time, approximately one out of every 25 hospitalized patients in the United States has an HAI. These infections result in the loss of tens of thousands of lives each year.
Cleaning, disinfecting, and sanitizing all contribute to preventing infectious diseases. Cleaning removes dirt, allergens, germs and impurities from a surface, but doesn’t necessarily kill germs. Sanitizing reduces the number of germs on a surface to a safe level, as determined by public health standards or requirements. Disinfecting lowers the risk of spreading infection by using chemicals to kill germs. Sanitizing can work by either cleaning or disinfecting surfaces to lower the risk of spreading infection.
Disinfecting or sanitizing in an institutional setting requires a level of cleaning effectiveness that ensures bacteria and viruses are not only eliminated, but also that the cleaned surface is rendered incapable of bacterial and viral growth. The Association for Professionals in Infection Control and Epidemiology (APIC) defines disinfection as a process that eliminates many or all microorganisms except spores.
According to APIC, there are three levels of disinfection:
- High-level disinfection destroys all microorganisms, with the exception of high numbers of bacterial spores.
- Intermediate disinfection inactivates M. tuberculosis, vegetative bacteria, most viruses and most fungi, but does not necessarily kill bacterial spores.
- Low-level disinfection can kill most bacteria, some viruses, and some fungi, but it cannot be relied on to kill resistant microorganisms (e.g., M. tuberculosis or bacterial spores).
For disinfection to work, proper contact time and dilution must be followed to improve the effectiveness of the antimicrobial agents, such as quaternary ammonium compounds, or ‘quats.’ Quats work by binding to bacterial membranes and breaking them down, thus destroying the cell. In order to be effective, quats need to be in contact with the surface being disinfected or sanitized for a period of time so they can kill all of the microorganisms present on the surface.
Optimizing Quats with Glucopon
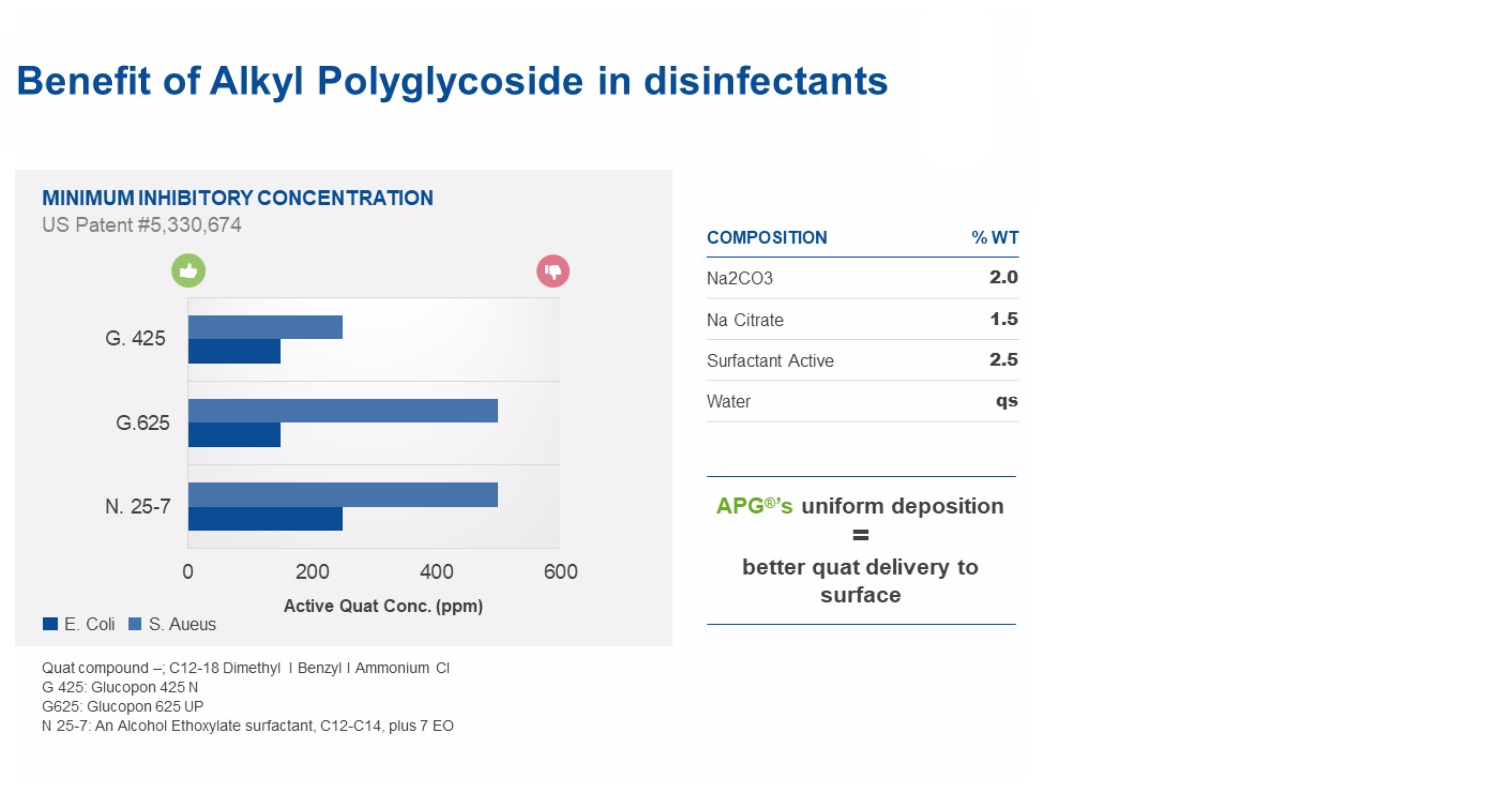
Typical alcohol ethoxylate surfactants have been shown to reduce the effectiveness of quats, meaning more of the surfactant must be present to kill the bacteria. However, similar behavior is not necessarily seen with Glucopon®, a line of alkyl polyglycoside surfactants. We believe that it is due to the ability of these APGs to provide a uniform deposition of quats on surfaces, that the amount of surfactant needed for high disinfection rates is reduced.
The graph, “Benefit of Alkyl Polyglycoside,” shows that both Glucopon 425 N and Glucopon 625 UP allow you to use less active quats to kill both gram-positive and gram-negative bacteria when compared to an alcohol ethoxylate surfactant. This is due to the active ingredients being more uniformly deposited.
Superior Surface Cleaning with Lutensol
For highly effective surface cleaning without the use of now-banned, Alkyl Phenol Ethoxylates (APEO), BASF’s Lutensol® types are a high-performing option. As shown in the performance graph comparing Lutensol XP/XL and APEO, both Lutensol XL and Lutensol XP perform at a higher level than APEOs, while also meeting the Safer Choice Standard.

